Cancer: From Access to Care to the Complexity of Data In Oncology and The Promise of Genomics
Cancer is a data rich diagnosis, consequently we need improved interoperability and a lot of AI moving forward. Not to mention smart approaches to enable access to novel treatments.
From an airplane view, developments in oncology are a rollercoaster of sorrow and pain, but also exciting new findings and hope. The absolute number of people diagnosed with cancer rose by around 50% in Europe over the past 20 years. However, the number of deaths only increased by 20%. Statistics show we’re making great strides in survival, treatments, and early screenings. For many patients, cancer is not a death sentence anymore. But there are many IFs.
Cancer has a higher incidence as we age due to an increased error rate in the cell multiplication process. It is these errors that can lead to harmful mutations. While cancer prevention approaches are well documented and based on behavioral, environmental, and lifestyle factors such as smoking, obesity, alcohol consumption, poor sleeping patterns, and stress, it seems we’re not acting upon the knowledge about prevention very well on the population level. Very recent research in Nature shows an increasing incidence of cancer in patients younger than 50 years.
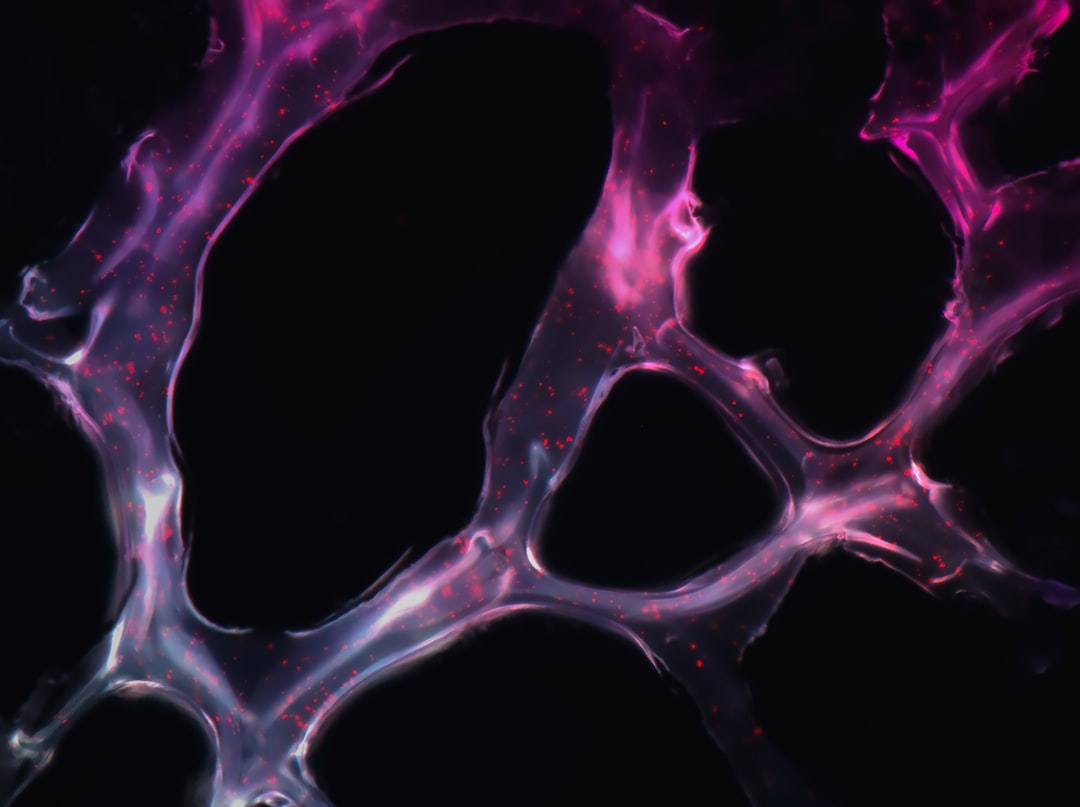
Genomics of cancer
Roughly 10% of all cancer patients have actionable mutations for which the Pharmaceutical industry has already found targeted precision therapies. However, even if a patient has an identified actionable mutation, only 30-40% of these patients will respond to targeted therapies.
Advancements in sequencing technology are decreasing the prices of genetic and genomic testing, making more samples available for analysis and new scientific findings. On the other hand, this is also driving an increasing demand for experts with the knowledge to interpret all this data and help translate it into clinical practice.
While there have been many new discoveries since the end of the Human Genome Project in 2003, we still have a long way to go in decoding human health and cancer genomics. Apart from previously mentioned actionable mutations, some variants are of unknown significance and must be continuously re-evaluated with new scientific discoveries. This makes the management of genomics data extremely energy-consuming and demanding.
There’s another caveat: If we’re increasingly tailoring therapies to an individual, the existing model of clinical trials becomes unsustainable because it’s impossible to test a drug on a cohort of patients when that drug is only designed for one particular individual, said Tuvik Beker, CEO of Pangea Biomed.
In the Cancer Series on Faces of Digital Health, five experts from France, UK, Israel and Canada explain:
What can genomics and data science tell us today about cancer (Episode 2 with Xose M. Fernandez, genomicist, former Chief Data Officer at Institute Curie in France),
How is AI trying to decode environmental factors sustaining or destroying tumor cells? This could aid in finding new treatments and design recommendations for more effective use of existing ones (Episode 3 with Tuvik Beker, CEO of Pangea Biomed in Israel),
What is the availability of therapies in the US and Canada (Episode 1 with David J. Stewart, MD, FRCPC, Professor of Medicine in the Division of Medical Oncology at the University of Ottawa and The Ottawa Hospital),
When patients survive cancer, what happens to their quality of life and what still needs to change to help them and their financial independence (Episode 4 with Dr. Françoise Meunier, member of the Belgian Royal Academy of Medicine, former Director General of European Organisation for Research and Treatment of Cancer, and a Scientific Member of the European Cancer Patient Coalition),
How does a data-first approach in the largest oncology center in Europe look like (Episode 5 with Phil Bottomley, EHR Strategic Lead at The Christie NHS Foundation Trust).
Access to drugs
At the moment, investments in drug development are high, and if a patient has cancer with actionable mutations, there are extremely effective precision therapies available on the market. But not necessarily accessible to every patient. David J. Stewart has been working in the US and Canada for decades. Comparing the two systems, he observes that doctors in the US market can offer patients all the latest drugs, but because US healthcare is a free market, these drugs can get extremely expensive very quickly because of co-pays and deductibles.
On the other hand, in Canada, coverage of oncology therapies is better, but the newest drugs arrive on the market with a delay. “It takes an average of 12 years to bring a new drug from discovery to marketing. What scares me the most in cancer care is that people will decide that things are so expensive that they can't afford to pay for them. And if that happens, then progress halts. If a company can't sell a drug, then they're not gonna invest in it.
In the US, if people have Medicare, most of the cost may be covered. They've got good insurance. But if there are large co-pays, then with very expensive drugs, even if 80% of the price is covered, the therapy is still very expensive. If the patient does not have insurance, then it's very difficult to pay for the medications.
Healthcare costs are responsible for a very large number of personal bankruptcies in the United States because of the cost of new drugs. In Canada, the way it works is that, for example, in Ontario, where I'm based, the government will pay for any intravenous chemotherapy or for oral therapies for anybody with cancer. They'll pay for these drugs for people over the age of 65 if they approve them, but not for people under the age of 65. Some of the new oral therapies are very expensive. There are ways of getting around that. Also, some people do have very good insurance as well. Not infrequently, the insurance will cover 80%, and the drug company will forgive the other 20% and cover it. So that helps.
But the big problem that we've got in Canada is that it can be a year and a half on average after Canada approves new drugs. Companies do not apply to Canada until an average of eight to 10 months after applying to the United States or Europe, simply because Canada is a much smaller market. The United States has 330 million people. The European Medicines Agency in Europe negotiates on behalf of about 500 million people. Canada has a population of about 35 million people,” said David J. Stewart. He recently published a book A sort primer on Why Cancer Still Sucks ... plus the crabby details, in which he tries to answer common questions patients might have, regarding cancer, treatment and accessibility.
Research starts with data.
Upward of 60 gene and cell therapies are projected to reach regulatory approval in the U.S. by 2030, according to the MIT NEWDIGS collaborative.
Medical advances are driven by research, and quality research requires quality data. In episode 5, we dive into the digital strategy of the largest single-site cancer center in Europe and the biggest chemotherapy center in the UK - The Christie NHS Foundation Trust.
The institution runs 650 clinical trials at any given time. It recently went live with a new electronic Patient Reported Outcome Measures (ePROMs) service helping to connect patients with the hospital trust through their cancer journey. As explained by Phil Bottomley, EHR Strategic Lead at The Christie NHS Foundation Trust, the digitization of ePROMs is only the beginning of the digitalization process of over 600 clinical forms used in the hospital.
The hospital’s digital transformation strategy is based on a data-first approach, ensuring that the used data models enable the creation of a longitudinal record. “When the data component is solved, it’s not that important where the data comes from,” said Phil Bottomley to the question of how the hospital is tackling data capture in the increasingly virtually supported care, which enables decentralized clinical trials.
For data organization, The Christie is basing its transformation on openEHR specification - a product and vendor-independent specification, striving to make data independent of any software provider.
Life after cancer is not normal.
Many patients survive cancer, and when results show that their disease is gone, they get told by their doctors that they can now finally go on with their lives. However, in reality, that’s often difficult. If they’re a part of the active population, they face several challenges on the job market or when they try to access loans.
In Europe, patient advocates have been fighting for the right to be forgotten for cancer patients for years. This is not related to the right to be forgotten mandated by GDPR. In cancer survivorship, the right to be forgotten relates to the fight to decrease the financial toxicity of a past cancer diagnosis.
Dr. Françoise Meunier, a member of the Belgian Royal Academy of Medicine, former Director General of European Organisation for Research and Treatment of Cancer, and a Scientific Member of the European Cancer Patient Coalition, has been at the forefront of advocating for the right to be forgotten across Europe. In Episode 4 of the cancer series, she explained the factors that impacted changes in France. France now mandates that past cancer diagnoses should be ignored after an individual has been cancer free for five years. This is a recently decreased timeframe from the previously determined 10-year period.
By 2024 a code of conduct about the right to be forgotten should be available on the European level. “It is not binding, it consists of guidelines and recommendations, which I don't consider strong enough, but it is the first step. And I think the more years pass, like in France, the more people will be confident that it is not a catastrophic situation,” Françoise Meunier said. “To my knowledge, there is no single French insurance company that became bankrupt because of the initiation of the right to be forgotten; on the contrary, now, they themselves, in France the largest insurer, decided to withdraw the medical questionnaire. So it shows that it is effective and it doesn't affect financial success.”