Advancing Digital Transformation Requires Strategic Planning and Immeasurable Patience
The secret to successful healthcare digitalizations is in leadership and knowing the "how" to digital maturity. We're in the middle of the path to the European Health Data Space (EHDS).
This is a monthly newsletter of Faces of Digital Health - a podcast that explores the diversity of healthcare systems and healthcare innovation worldwide. Interviews with policymakers, entrepreneurs, and clinicians provide the listeners with insights into market specifics, go-to-market strategies, barriers to success, characteristics of different healthcare systems, challenges of healthcare systems, and access to healthcare. Find out more on the website, tune in on Spotify or iTunes.
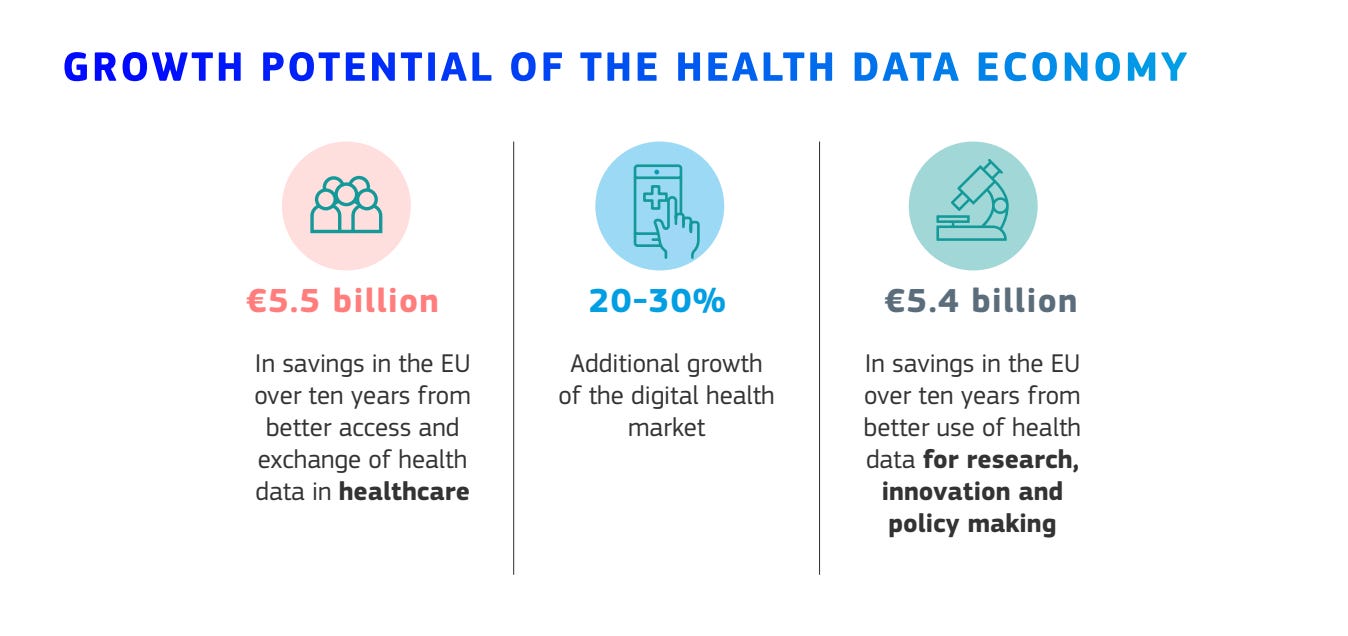
Ideal healthcare data universe is clear: having the right data at the right time, regardless of where patients seek care. This involves seamless data flow with robust privacy protections, ensuring sensitive information remains secure. The European Health Data Space (EHDS) aims to achieve this through several projects in the past and present exploring ways to unify diverse data standards and healthcare IT systems. The ultimate goals: optimizing healthcare and contributing to its sustainability.
Source: EHDS Factsheet.
Why is this so hard to achieve in real life?
Fragmentation in European Healthcare
Europe’s healthcare landscape is a patchwork of 27 countries, each with a different language, financing, and reimbursement schemes. Larger countries are further divided into autonomous regions, complicating healthcare IT architecture. Patients often face confusion when seeking care outside their regions due to inconsistent digital systems.
For example, Italy has 20 regions with varying levels of digitalization. Northern regions like Lombardy are advanced, while southern areas lag behind. As Marco Foracchia, CIO of Local Health Unit in the Emilia Region, IRCCS, describes, patients struggle to make appointments as each region uses its own digital tools.
Healthcare providers may be digitized, but they are not always connected. Historically, software procurement has been fragmented, with institutions independently deciding on solutions without broader regulatory mandates for standardization. When buying software to date, healthcare institutions have often seemed as of 3 year olds who say “I will decide for myself” and potentially “I don’t to have what Mary has".
Up until recently it was legally forbidden to share data in the Netherlands. With a new law two years ago, the direction has shifted and is aligned with the current broader mindset across the world, to create ecosystems where data follows patients.
Decisions in the past created legacy systems, which left patient data fragmented among several patient portals for different services patients are using. Slowly however, we are seeing consolidation progress on regional levels.
Case Study: OneLondon
Though the UK is no longer in the EU, its healthcare data consolidation efforts offer valuable lessons. In London (population: 8.8 million), 24 different EHR systems exist. The OneLondon project, launched in 2018, aimed to connect 35 NHS Foundation Trusts across five Integrated Care Systems.
Since its inception in 2018, OneLondon has evolved significantly, with increased data-sharing capabilities that now extend beyond London. This interconnected system allows various healthcare providers to access critical patient data at the point of care, facilitating better-informed treatment decisions.
The bigger picture is care that’s integrated not just between healthcare institution but social care as well. Many police interventions are related to mental health issues, and police is not equipped to dela with them properly.
Progress happens one segment at a time
Improving interoperability in London is incremental. To support end-of-life patients, OneLondon centralized urgent care plans on a platform accessible to all EHRs. Additional care plans are being introduced based on these learnings.
Queen’s University Belfast did an independent economic evaluation of the London Care Record, and found that based on 27 million uses of the London Care Record (up to March 2023), the value of time saved is estimated to £2.1 million per month, with 20,000 hours per month saved.
Public trust is everything
Interoperability projects are very technical and hard to translate into lay language. But in the end it’s the human factor that is essential for success. Luke Readman, the CIO of OneLondon says building public trust has been central to OneLondon’s success. The project engaged in annual public consultations to understand and align with the public’s expectations for data usage and privacy. This inclusive approach helped strengthen public support and confidence in the system.
Similarly, before France designed their digital health ambitions and investments, they did a thorough on the ground research to see the differences between regions and populations and also understand what people expect from healthcare digitalization.
The Small Countries Problem
To support EHDS, large countries first need to set national strategies to harmonize regional data with EHDS requirements. On the opposite end, smaller countries have a different problem: lack of choice.
Healthcare IT solutions aren’t like consumer products you can order from wherever to wherever. Healthcare IT vendors may deprioritize smaller markets due to the high cost of localization and low scalability. This lack of competition can result in outdated systems, as vendors have little incentive to modernize their offerings.
End of data standards wars?
On the up side it seems that collaboration is coming in the front row of data standards debates and data standards bodies. The Annual International openEHR conference in November 2024 showcased leaders from Karolinska University Hospital, Catalonia region, University Hospital Basel, and vendors such as AWS advocated for combining openEHR (for clinically granular data storage) with FHIR (for messaging).
The focus has shifted from debating which standard is superior to exploring how standards can work together.
Starting at the source
Regional and national perspective are a few levels above the source of data capture challenges which start in healthcare institutions. In the era of cyberattacks being a weekly occurrence, AI, medical devices and digital health rapidly advancing, it may seem easier and cheaper for healthcare institutions to stick to paper. In many cases in Europe, they still do. Software implementations take years of time and millions of euros.
Several challenge are present in this process for vendors and providers:
Providers may have unrealistic expectations or lack clarity on their needs.
Vendor claims in tenders are difficult to validate.
To avoid incorrect purchases, healthcare providers are embedding clauses in contracts that stipulate payment is made only after successful installation. This puts vendors in a tough spot of planning their revenue, especially since delays are common in implementations.
Helping hand in digital transformation
The EU’s Resilience and Reconstruction Program (PNRR) has driven funding and deadlines for nationwide EHR implementations. Ministries had to design strategies, designate funding, write tenders. In 2026, we will see the successes, failures and EU funding that will need to be returned if implementations are not in place.
One helping hand hospitals and countries can use when considering where to even begin with healthcare digitalization and what to invest in first, are HIMSS maturity models. These are self-assessment questionnaires, that enable hospitals to benchmark their current capabilities and outline their roadmap for digital transformation, aligned with global standards. With this they can enhance decision-making for procurement and strategy, and avoid installing the wrong solution that will be hard to replace. Before Germany divided 4 billion euros to hospitals, they assembled a DigitalRadar project. Among other things, they assessed the digital maturity of hospitals with 65% of the evaluation based on HIMSS EMRAM criteria.
HIMSS offers six maturity models, each focusing on different aspects like EMR adoption, infrastructure, and community care. Each model has seven stages helping hospitals understand where they are. Recognition of the highest levels of digitization (e.g., Stage 6 or 7) involves on-site assessments by HIMSS experts.
At HIMSS Europe a dedicated track called Digital Maturity Roadmaps will give hospital an national representatives an opportunity to meet and learn from hospitals across EMEA and beyond about their digital transformation journeys.
In 20 years ….
The EHDS framework for cross-border data exchange and secondary data use has spurred necessary changes across Europe. Even in smaller countries vendors will need to upgrade their solutions to meet European expectations.
We’re still far away from the idea of the perfect healthcare data universe described in the beginning. Progress being made will be measurable in the next 10 to 20 years.