How are Germany, Slovenia and the Netherlands Approaching Healthcare Digitalization?
Countries across Europe are ambitiously pursuing digitalization efforts. How are they doing?
This is a monthly newsletter of Faces of Digital Health - a podcast that explores the diversity of healthcare systems and healthcare innovation worldwide. Interviews with policymakers, entrepreneurs, and clinicians provide the listeners with insights into market specifics, go-to-market strategies, barriers to success, characteristics of different healthcare systems, challenges of healthcare systems, and access to healthcare. Find out more on the website, tune in on Spotify or iTunes.
If it seems that the world is moving faster and faster with the rapid evolution of AI and other technologies, the digitalization of healthcare infrastructure is not changing with that speed. However, countries across Europe have been strategizing and investing heavily in digitalization efforts since the pandemic.
On top of that, the European Health Data Space legal framework created the basis for enabling the secondary use of data on the EU level, and some countries in the European Union are already leveraging the MyHealth@EU infrastructure for cross-border health information access and services such as ePrescriptions.
In 2023, Germany, Netherlands, and Slovenia have published their new digitalization strategies.
All three countries differ a lot in almost everything - size, population, % of GDP expenditure for healthcare, healthcare system structure, and digital maturity. So what are their key goals for the future digital transformation?
Tune in or read the summary.
Slovenia: Consolidated national eHealth infrastructure
Slovenia is not often… actually never mentioned as an interesting country from the digital health perspective. Because the market is small, innovators don’t perceive it as an interesting target market. Consequently, solutions such as digital therapeutics are not on top of the minds of health insurance providers.
Slovenian healthcare services are paid from the centralized insurance fund, run by the Health Insurance Institute of Slovenia. It is mandatory for all employed individuals to make contributions to the insurance fund from their salaries. In addition, people pay an additional 35 euros of complementary health insurance which is not obligatory, but without it, individuals risk high co-pays when utilizing health services.
The national eHealth infrastructure, which is based on the openEHR data platform, is managed by the National Health Institute. “By today, 99.5% of providers are using ePrescription. There are basically no paper prescription forms anymore. With the new digital health law, we are also forcing all healthcare providers - private or public - to connect to the national EHR. In case of lack of compliance, the manager of the healthcare provider will get a fine,” explained Alenka Kolar, Acting Director-General of the Directorate for Digitalisation in Healthcare at the Ministry of Health Slovenia.
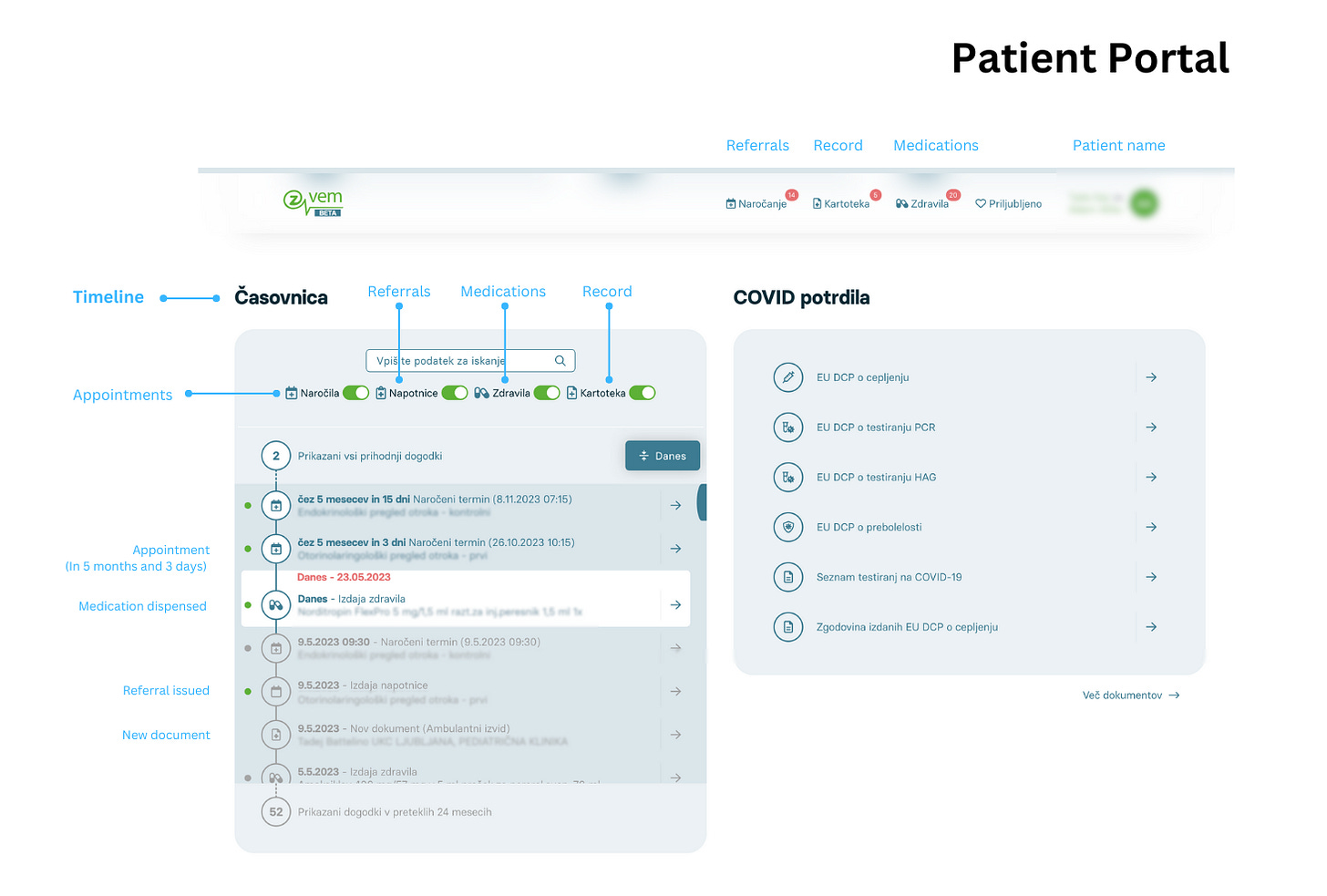
Apart from ePrescriptions, patients can access their EHR via the patient portal, which contains main information related to secondary and tertiary care: they can see all the eReferrals for specialist appointments, a list of prescriptions they have already picked up or still need to pick up in the pharmacy, pdfs of their discharge letters, and a timeline of scheduled medical appointments - regardless of the healthcare provider.
On the primary care level, GPs still use their own separate systems for communication with patients, and the systems differ from GP office to GP office. However, this is aimed to be unified under the new strategy.
One of the main goals for Slovenia is to further advance its digital services and improve the investment in healthcare IT. At present, out of all the gathered contributions for health insurance, 0.5% goes to healthcare IT. The objective of the new digital health strategy is to progressively increase the allocated funding to 6% of the national healthcare insurance expenditure.
Netherlands: National interoperability by 2035
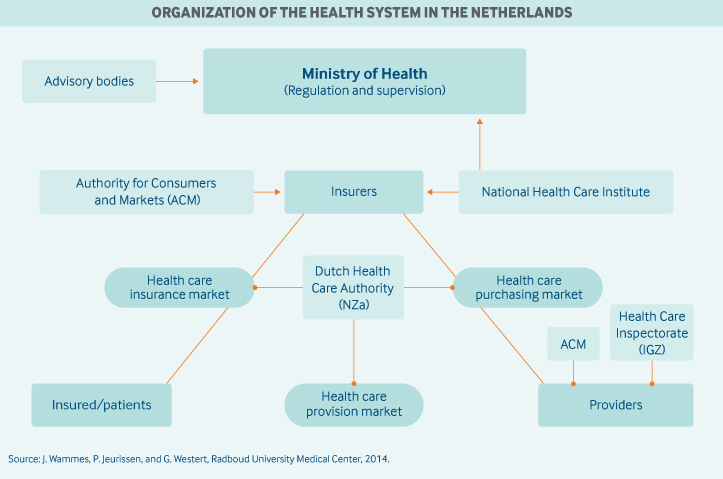
In the Netherlands, everybody is obliged to buy health insurance, but they can choose from 5 main health insurance companies. This creates a market dynamic where insurance companies and healthcare providers compete for patients and healthcare provision.
Source: The Commonwealth Fund
The Dutch healthcare providers are highly digitized and hospitals spend a lot of money for IT. Unfortunately, healthcare data is siloed in different institutions. “We have high numbers of IT personnel in our hospitals. But we have a private system of healthcare. There are 45,000 diverse healthcare institutions including GPs. The hospitals have a lot of IT personel and knowledge. At the same time, the other participants in the healthcare system don't have access to the knowledge. Between 80% and 90% of all providers offer patients digital access to their medical files. But these are single portals. One of our questions for the next years is how are we going to use the knowledge and the capacity of the hospitals to also get other sections of the healthcare system digitalized,” said Bianca Rouwenhorst, CIO at the Ministry of Health, Welfare, and Sports in the Netherlands.
The reason for the lack of data fluidity among institutions lies in a law enforced in 2011, which forbade the creation of a national healthcare infrastructure. After 12 years, this is about to change. “A few years ago healthcare providers urged the government to take more control over the interoperability problem. Many activities have been done in the last two years and this resulted in the unanimous agreement in the Senate to support the Electronic Data Exchange in Healthcare law this year. Our goal is to create a data-centric network with optimal data availability to meet the needs of healthcare providers, patients, and researchers. At this moment, we are focusing on language standardization, using FHIR and open APIs in healthcare to facilitate data exchange between healthcare providers and patrons. Our goal is to achieve data interoperability and data consolidation by 2035,” says Bianca Rouwenhorst.
Germany: 1% of people using EHRs
The challenges with healthcare digitalization and reforms are complex, due to various data privacy concerns, the digital divide, integration issues among different healthcare information systems, and different complexities of healthcare systems.
With 83 million people, Germany is a large country, divided into 16 federal states. The federal government is responsible for the overall healthcare provision and has limited power. That’s only a part of the complexity. “We have several layers of complexity and responsibilities. The federal government is responsible for the overall healthcare provision. Then we have the lender who is responsible for the financing of hospitals, but not the outpatient treatment. And this is the political responsibility. In addition to this, we have a layer of self-government, which means that our statutory health insurance funds and the physician's organizations, the hospital organizations negotiate a lot with each other. So basically when we make a law on the federal level only very few have a direct impact,” explained Sebastian Zilch, Head of e-Health, Gematik & Telematics Infrastructure at the German Federal Ministry of Health.
There are over 100 health insurance companies in Germany. 90% of the population is insured through public insurance, 10% through private insurance.
From the digitalization point of view, people insured through the public system are at an advantage, because all of the healthcare digitalization regulation applies to the public system. But there is still a long way to go even for them to benefit from the existing infrastructure.
National healthcare digitalization is the responsibility of Gematik - a dedicated national agency, which has only been under federal control for the last 3 years. Gematik has established a significant amount of infrastructure, but the difficulty lies in its practical application in the real world.“I think we have the most relevant players connected to the common secure infrastructure. We also have a lot of applications, for example, e-prescriptions and electronic health records. But the big problem is this is not being used. Less than 1% of people are using our electronic health records. This led to a very broad consensus in this country, that we need to go ahead with the digital transformation to make healthcare future, and resulted in the strategy we published in March,” says Sebastian Zilch.
Two laws are being drafted to support the digital transformation efforts. Electronic health records won’t be an opt-in option anymore, citizens will have to actively opt out in case they would wish to avoid having an electronic medical record. Similarly, healthcare providers will be obliged to send information to the electronic infrastructure. “We want everything that's being prescribed automatically transferred in the health record, so the physicians actually have reason to use the EHR and it becomes part of the care process. Right now it's an add-on. And it's understandable that nobody really uses it. For all this to work, we also need to make usage of e-prescription compulsory, so there will be penalties if people don't use it. There's a second law in the pipeline for the use of data for research and we hope that both will actually be in effect January next year,” said Sebastian Zilch.
EHDS
Considering the existing challenges with data fluidity and interoperability within countries, how feasible is it to anticipate timely implementations of the European regulatory framework that would be visible to people in the near future? All speakers are happy that the European legal framework exists, as they perceive it as the catalyst that will facilitate the fulfillment of their respective national plans.
Future plans
One big change is expected by the ministries: hospitals must begin considering IT as an integral component of healthcare provision. Consequently, the costs associated with digital services and tools will need to be incorporated into the price of healthcare service provision.
In its new healthcare digitalization strategy, Slovenia plans to gradually expand the annual budget for eHealth from 6 million euros per year to 80 million euros per year, and gradually increase the % of the healthcare budget for IT to 6%. Additional 83 million euros are available from the EU recovery fund and need to be used by the end of 2026. The challenge is the low number of healthcare IT staff in healthcare. To enhance efficiency, the Slovenian ministry is striving to create a national company that will consolidate the existing personnel into a unified group, supplemented by the recruitment of additional staff members. “This is similar to Estonia, and I think Portugal has the same organization. We will deliver the infrastructure in a modular way. We will not develop one single big solution from one provider, but smaller modules put on the data level. And all the data should be organized by openEHR specifications,” said Alenka Kolar.
While Germany has a long way to go, a lot has happened in the past few years. For one thing, Germany has become the first country in the world that established a framework and system for the approval of digital therapeutics and their automatic reimbursement if the doctor prescribes them.
The DigitalRadar consortium, which includes HIMSS and other research and advisory partners, carried out the evaluation of the digital maturity of hospitals on behalf of Germany’s Federal Ministry of Health. 1600+ hospitals were included in the assessment and had the opportunity to apply for funding for digitalization projects. The average DigitalRadar Score is 33 out of a possible 100 points, and most hospitals (70%) scored between 23 and 44 points. 4,3 billion euros were available for digital transformation and by 2024 hospitals must provide evidence of implementing and effectively utilizing funded projects, or else they may be required to refund a portion of the funding.“We'll have to see what happens after because for years the hospital sector has been underfunded. We are currently in a huge structural reform of hospitals. So the hospital landscape is going to change. And with this, the financing of digitization will have to change, but we are in an early stage,” said Sebastian Zilch.
The Netherlands plans on spending 1,4 billion euros for healthcare digitalization by 2026. “With our new law, we defined five use cases that we are going to standardize by indeed the national Zibs common data model, and we are doing the same thing as Slovenia, which is to mandate hospital centers and GPs to give their data to the personal health care environments. When you get paid by the insurance company for giving care, then you also have to give your data otherwise you don't get paid. That's what we are going to mention in the legislation, and we are doing that for five use cases - the patient summary, the medication, and e-prescription, but also for a use case for elderly care,” mentioned Bianca Rouwenhorst.
For the full discussion, tune in to the podcast.