The Patient Perspective at HIMSS 2023
Patient-centricity is putting patients in a new light, but they still too often fall through the cracks.
There’s a great discrepancy between scientific knowledge and advancements in human-centered design, treatments, innovation in the digital health market, and the care we get when interacting with healthcare. The Patient Experience pre-conference forum at HIMSS 2023 - the largest global conference on healthcare digitalization, which this year attracted 35.000 people to Chicago, focused on all things patients: from digital experience, human-centered care, trust, virtual care, and patient safety.
From many perspectives, patients have never in history been in a better position:
we’re talking more about empathy and partnership in the physician-doctor relationship,
we can find a lot of information online, and searching for answers is getting increasingly easier with AI,
we have more and more point-of-care diagnostic devices and monitoring wearables that allow us to take control of our health.
From many perspectives, the possibilities we have today, compared to even ten years ago, are admirable. However:
it can still take up to ten years for a patient to be diagnosed with the right mental health disorder or a rare disease,
patients are still struggling to consolidate and access all their medical data,
as patients, we are still very vulnerable and could use help remembering and understanding all the doctor’s information we get and how our care is going to look like.
“We don’t talk enough about shame in the patient experience discussions. Patients need to feel safe and that the healthcare system has their back,” said Aaron Miri, Senior Vice President and Chief Digital & Information Officer at Baptist Health, in his opening keynote at the pre-conference forum.
Baptist Health currently uses five mobile apps for its patients, which were developed based on the detected patient needs. As mentioned by Aaron Miri, listening to patients and providing them with what they ask for and what addresses their needs helps with efficiency. “‘There’s an app for that’ is being replaced with ‘there’s an AI model for that’,” he mentioned.
Red flags, data blocking, and other challenges patients face
The patient experience is closely related to patient safety.
“In 1991 patient harm stopped being seen as part of everyday medicine, where we said - you save some, you harm some. Patient safety was recognized as a serious challenge. Unfortunately, we have not made much progress in patient safety,” said Eyal Zimlihman, Chief Transformation Officer and Chief Innovation Officer at Sheba Medical Center in Israel.
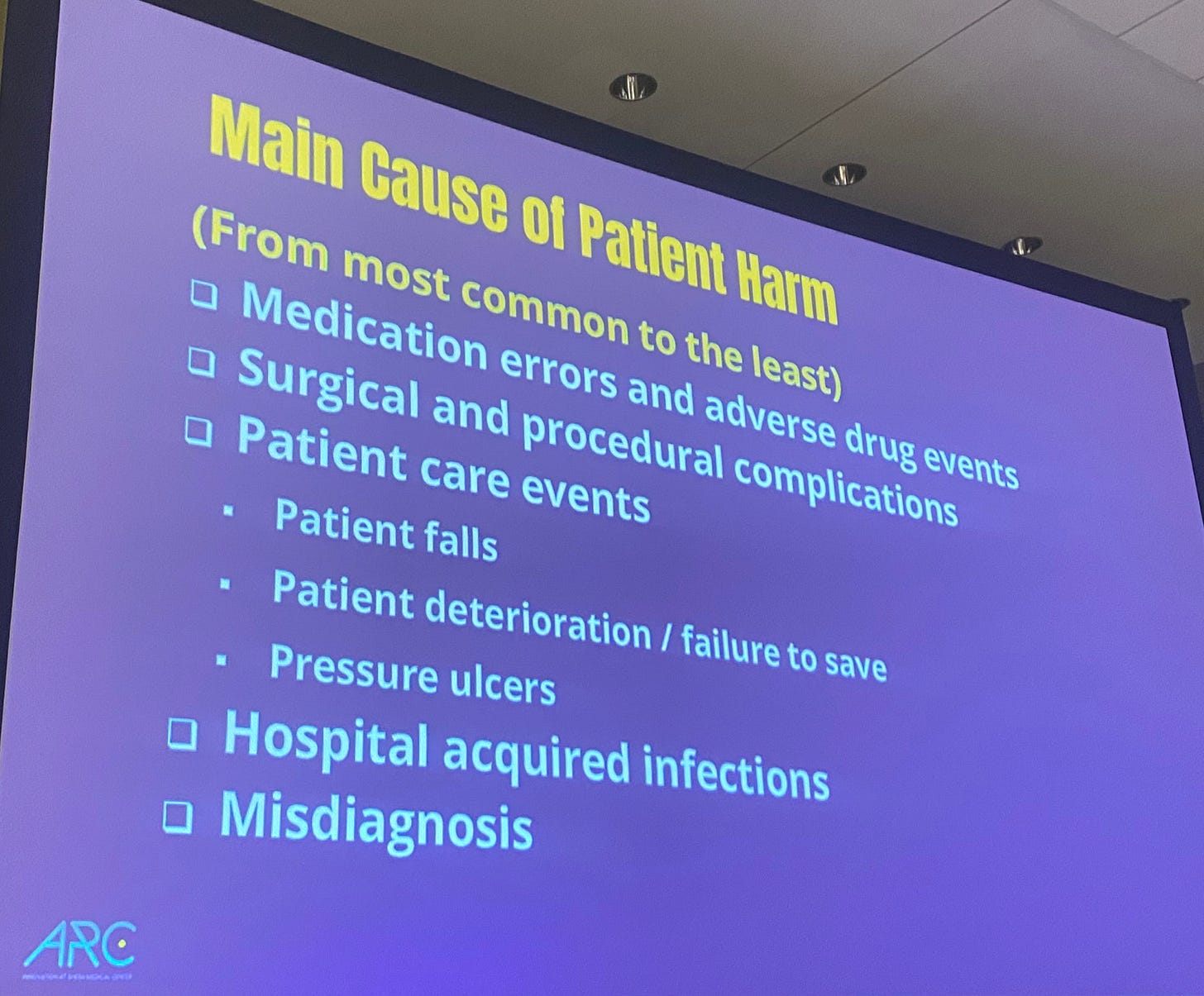
The statistics in this regard are clear: the main cause of patient harm remains medication errors, followed by surgical and procedural complications, patient care events, hospital-acquired infections, and misdiagnosis.
Side recommendation: if you haven’t yet, watch the documentary (OVER)DOSE - How Can We Prevent Medication Errors. Trailer below:
Movie, adapted for audio:
It’s one thing to talk about workflows, processes, and statistics, but quite another to give a name and a face to the consequences of poor communication, prejudice, and harm patients experience in healthcare. The patient advocate panel discussion was a reality check on healthcare access, inclusion, and challenges with digitalization.
While everyone is trying to use technology for better outcomes and work optimization, patient advocates raised several concerns, such as:
How could patients know if doctors use the best technology? Could patients choose which algorithms doctors should use, based on quality control ranking, if that existed?
How can we use EHR data for AI when medical records are full of errors, with patients not having a chance to review and correct their records?
How can we prevent algorithms from being dangerous when they’re already being used to deny insurance claims in bulk, which increases the workload of healthcare providers, patients, and their advocates, if they try to appeal. “Doctors are burned out, well patients are burned out too,” said Grace Cordovano, Chief Executive Officer and Board Certified Patient Advocate People with Empathy. She pointed at several red flags patients experience daily, such as:
1. Patients must sign consent forms that do nothing but protect providers. Patients are given an electronic empty sign box without being aware, let alone well-informed what they are signing.
2. Resistance to allowing family members to communicate with physicians.
3. Labels: patients still report feeling judged based on the perception that they will not be able to pay for treatment.
From left to right: Grace Cordovano, Christine Von Raesfeld, Greg O'Neill, Bradley Schwartz.
”Trust is a moving target: we used to trust doctors with bloodletting to treat infections,” said Greg O’Neill, - Director, Patient and Family Health Education, ChristianaCare. “We have a plethora of data… you bet. How much of it is accurate? How much of it is understandable to the average person?” he mentioned.
The patient advocated urged to better communication and access to medical records, which should be embraced, not feared. “We need to learn from marketing: they marvel at connecting with us. Healthcare needs to learn how to connect with patients better: more clarity, less jargon,” also said Greg O’Neill.
Virtual and Remote All The Way… But Not Everywhere
In South Korea, telemedicine will not become a standard of care any time soon, in fact, it will soon be illegal as it was before the pandemic. “The pandemic had opened a window forward to telemedicine, and remote healthcare services have been widely expanded. Approximately 20% of the total care cases, with the majority being primary care clinics, were done by physicians contacting patients by telephone, and patients could receive transcriptions electronically,” explained Mira Kang, Vice Chief Medical Information Officer at the Samsung Medical Center in South Korea, during a panel discussion on virtual care.
The temporary allowance by the infection prevention law is likely to be forbidden within a month because the COVID-19 pandemic has ended. “Remote patient monitoring or teleconsultation between physicians is only allowed in special cases for the prisoners or the Coast Guard dispatched to the Dokdo island 153 miles away from the mainland, or sailors on the oceans,” Mira Kang, additionally mentioned (Tune in a short discussion below).
In the US healthcare system, on the other hand, there’s no question that hospital at-home and extensive remote monitoring are only moving forward. Rasu Shrestha is Chief Innovation and Commercialization Officer, Executive Vice President at Advocate Health - US healthcare system that has built the so-far largest remote-monitoring program in the US. As Shrestha has said several times by now, hospitals at home and remote monitoring “are shining the light on the dark side of the moon,” which is what patient homes represented up until now. After patients leave the hospital, they fall in the dark from the provider’s perspective; there’s no clue what is happening at home until patients return to the hospital, often to be re-admitted due to a deteriorating health state.
Remote monitoring has several positive sides: it can warn healthcare providers about a potential complication in time, it might detect abnormalities faster, and trigger interventions that prevent health complications for patients. It’s more convenient if patients receive care at home instead of making appointments, especially if they live in rural areas and need to drive for hours to reach their healthcare provider.
Trust, Transparency, and Education
While the need might be the greatest in rural areas, virtual care is not necessarily accepted with open hands, was mentioned in a panel about virtual care. Patients there might be more conservative and suspicious about data gathering and their privacy said Brad Reimer, Chief Information Officer at Sanford Health, the largest rural health system in the US, which serves more than 1.5 million patients.
From left to right: Tjasa Zajc, Brad Reimer, Mira Kang, Shannon S. Crotwell.
There’s another problem with remote monitoring: it might not be calming and reassuring for all patients: for some, it may be extremely anxiety-inducing when their results aren’t good (even if the high blood pressure is caused by the fact that the patient measured it before taking medications), shared Shannon S. Crotwell - Program Coordinator within Adult Cardiac Surgery at Atrium Health.
Arming clinicians and patients with as much information as possible about data, privacy, data gathering, and the consequences might be crucial for virtual care to succeed.
Where are we with diversity and inclusion?
Many of these issues relate to challenges with diversity and inclusion, topics that are on top of the discourse in healthcare, especially in the US. Diversity and inclusion relate to human-centered design, patient inclusion, leadership, tackling inequities, having diverse management and executive boards, and more.
While at HIMSS 2023, I asked some of the 2023 HIMSS Most Influential Women in Health IT Changemaker Award recipients where they see the greatest needs and challenges to improve diversity and inclusion and why this matters if we want to advance healthcare for all:
“A lot of times, we find that the solutions are done without the end user in mind, without having that participatory piece. And as a result, the solutions are not what's needed, or they're not used,” emphasized Victoria Tiase, PhD, RN-BC, FAMIA, FNAP, FAAN Strategic Director Digital Health, Assistant Professor of Biomedical Informatics, University of Utah, School of Medicine Salt Lake City, Utah, United States.
“We must be able to tackle the needs of the most vulnerable in order to be able to say that we actually achieve health equity,” said Anca del Rio, MSPH President EIT Health Alumni, European Institute of Innovation and Technology Zurich, Switzerland.
“Many times, the way trust is established is when you see somebody talking to you who's just like, you know. Whether it's the same gender or whether it's the same race and ethnicity,” said Janis Curtis, MSPH, MA Associate Director, Clinical Data Research Networks, Duke Health School of Medicine, Clinical Translational Science Institute Durham, North Carolina, United States, who also pointed to the digital divide. “If anything, we learned that underserved populations are not being reached with our digital technology. Some people, especially in rural areas or in low economic areas, don't have the technology. So trying to get the clinicians to say, if you really want to get to that population, you need to figure out, ask them how they would like to be communicated with. Is it via phone? Is it a house visit? Or something else?”
Joy Rios, MBA Founder | CEO | Host, HIT Like a Girl Podcast Baja California, Mexico, on why diversity is crucial for progress: “We should be changing policies; we need to be addressing topics from both government, private organizations and community levels. That trifecta of making sure that we're addressing complex problems. And that requires diversity, the diversity of thoughts.”
**The recipient of the award is also Gabriela Mustata Wilson, PhD, MSc, FHIMSS, SNAI, FIAHSI Professor and Founding Co-Director, Multi-Interprofessional Center for Health Informatics (MICHI), University of Texas at Arlington (UTA) Arlington, Texas, United States.
Congratulations to all the recipients.